GUELPH – The University of Guelph (U of G) is co-leading a $15-million initiative that has the potential to help Canada be better prepared for future pandemics.
“We were caught flat-footed the last time with COVID-19,” said U of G professor Lawrence Goodridge, director of the Canadian Research Institute for Food Safety at the Ontario Agricultural College (OAC).
Goodridge, a professor in the university’s food science department, will co-direct the Integrated Network for the Surveillance of Pathogens: Increasing Resilience and capacity in Canada’s pandemic response (INSPIRE) with the University of Windsor’s Robert McKay.
The project received $12,940,731 from the Canada Biomedical Research Fund (CBRF) and $2,063,509 from the Biosciences Research Infrastructure Fund (BRIF).
The University of Guelph’s portion will include $3,237,557 from CBRF, and $624,946 from BRIF.Goodridge said the project aims to provide tools and knowledge needed to mitigate risks and increase the country’s capacity to respond effectively to future pandemics.
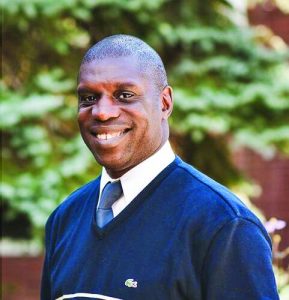
LAWRENCE
GOODRIDGE
Canada’s response during the COVID-19 pandemic could be improved upon, said Goodridge, describing as an example the supply chain disruptions that caused issues for the health care sector, among others.
“We couldn’t get PPE (personal protective equipment), we couldn’t get masks, we couldn’t get gloves,” he said. “We couldn’t get test kits for a while.”
Goodridge’s work involves wastewater surveillance, which he said the university has been actively involved in since prior to the pandemic.
Before COVID-19, he was focused on identifying food-borne pathogens such as E. coli, salmonella or listeria in wastewater, but he says the wastewater surveillance work “really took off” during the pandemic, when it was used to track outbreaks of the virus.
“We could detect COVID in wastewater approximately 10 to 14 days before people got sick,” Goodridge said.
The INSPIRE project builds on the wastewater surveillance network that developed during the pandemic, and will incorporate other emerging surveillance approaches in an effort to create an early-warning system for emerging infectious diseases.
Goodridge said social media monitoring is one of these emerging surveillance approaches, explaining that people will often share information about illness with their social media networks.
“When they get sick, people might not go to a hospital,” Goodridge said. “If you don’t go to the hospital, nobody knows you’re sick.”
Even when people do go to hospital, they might not test for a particular illness, and even if they do test, it can then take weeks before public health officials know about it, he said.
Goodridge’s team hopes to marry the more active surveillance of wastewater and social media monitoring with artificial intelligence technology to speed up the detection process so the biomanufacturing sector – which is involved in producing medicines and vaccines as well as foods – and the health sector can react more quickly to outbreaks.
Early detection of illness could help in multiple ways Goodridge said. It could reduce supply chain issues, help health care sectors mobilize human resources, or could even help stop an outbreak at the source.
“Then maybe we don’t need lockdowns,” said Goodridge, noting the irony of the work is that if it’s done well, the public won’t even know how necessary it is.
“If we do our work right, the public should never even know that there’s a problem,” he said.
Goodridge will be joined by U of G researchers Monica Cojocaru from the mathematics and statistics department at the College of Engineering and Physical Sciences (CEPS), Marc Habash from the School of Environmental Sciences with OAC, and Graham Taylor from the School of Engineering in CEPS.
The team also includes researchers from the University of Windsor, University of Waterloo, University of Toronto and York University, as well as partners at more than 30 academic, public, private and not-for-profit institutions.




